A cervical biopsy is a surgical procedure in which a small amount of tissue is removed from the cervix. The cervix is the lower, narrow end of the uterus located at the end of the vagina.
A cervical biopsy is usually performed if an abnormal tissue is found during a routine pelvic exam or Pap smear or Colposcopy. Abnormalities means the presence of the human papillomavirus (HPV), or cells that are precancerous. Certain types of HPV can put you at risk for developing cervical cancer.
A cervical biopsy can find precancerous cells and cervical cancer. Your doctor or gynecologist may also perform a cervical biopsy to diagnose or treat certain conditions, including genital warts or polyps (noncancerous growths) on the cervix.
Three different methods are used to remove tissue from your cervix:
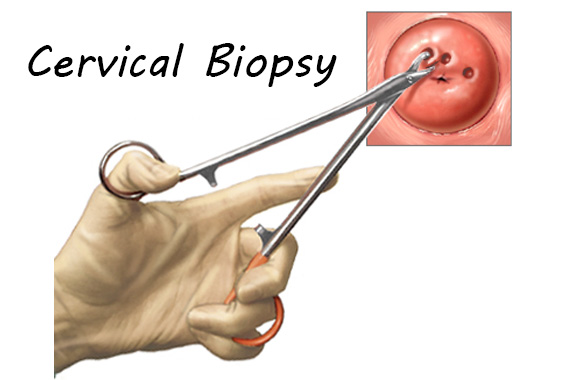
Punch biopsy:
In this method, small pieces of tissue are taken from the cervix with an instrument called “biopsy forceps.” Your cervix might be stained with a dye to make it easier for your doctor to see any abnormalities.
Cone biopsy:
This surgery uses a scalpel or laser to remove large, cone-shaped pieces of tissue from the cervix. You’ll be given a general anesthetic that will put you to sleep.
Endocervical curettage (ECC):
During this procedure, cells are removed from the endocervical canal (the area between the uterus and vagina). This is done with a hand-held instrument called a “curette.” It has a tip shaped like a small scoop or hook.
The type of procedure used will depend on the reason for your biopsy and your medical history.