Uterine Prolapse in women: Causes, Symptoms and Treatments
What is Uterine Prolapse?
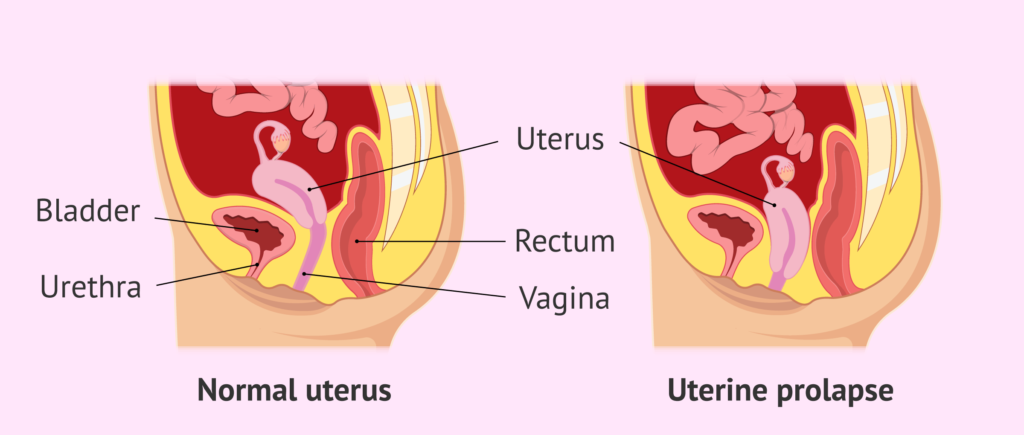
Uterine prolapse in women is a common condition that can occur as a person ages. It involves the weakening of the muscles and tissues that support the uterus, causing it to drop down into the vagina. While it can affect anyone born female, it is most common after menopause and in those who have had multiple vaginal births.
Who is at Risk for Uterine Prolapse?
Uterine prolapse in women primarily affects those who have had multiple vaginal births. Factors like aging, menopause, obesity and heavy lifting can also increase the risk. Women with a family history of pelvic floor disorders are more susceptible as well.
How Common is Pelvic Organ Descent?
Uterine prolapse is relatively common, particularly among older women. Studies suggest that nearly half of women who have given birth will experience some degree of prolapse in their lifetime. However, many cases go unreported because the symptoms can be mild.
How Serious is a Prolapsed Uterus?
The seriousness of uterine prolapse varies. While mild cases may cause little discomfort, severe prolapse can lead to significant pain and difficulty in daily activities. It can also affect bladder and bowel function, leading to incontinence and other complications.
Four Stages of Uterine Descent
There are four stages of uterine descent:
- Stage 1: The uterus drops slightly but remains within the vagina.
- Stage 2: The uterus descends to the vaginal opening.
- Stage 3: The uterus protrudes outside the vaginal opening.
- Stage 4: The entire uterus is outside the vagina.
What Causes Uterine Descent?
The primary cause of uterine prolapse in women is weakened pelvic floor muscles, which can result from:
- Vaginal childbirth
- Aging and menopause
- Chronic coughing or constipation
- Heavy lifting
- Obesity
Recognizing Symptoms of Uterine Prolapse
Symptoms of uterine prolapse can include:
- A feeling of heaviness or pulling in the pelvis
- Tissue protruding from the vagina
- Urinary problems, like incontinence or retention
- Difficulty with bowel movements
- Lower back pain
- Sexual discomfort
How is Uterine Prolapse Diagnosed?
To diagnose uterine prolapse, a healthcare provider will conduct a pelvic exam. Additional tests such as ultrasound or MRI, may be used to assess the severity of the prolapse and to plan the appropriate treatment.
Managing Uterine Prolapse: Treatment Choices
Treatment for uterine prolapse in women depends on the severity of the condition:
- Lifestyle changes: Weight loss, pelvic floor exercises (Kegels) and avoiding heavy lifting.
- Pessaries: Devices inserted into the vagina to support the uterus.
- Medications: Hormone therapy to strengthen pelvic muscles.
- Surgery: In severe cases, surgical options include uterine suspension or hysterectomy.
What Happens if Uterine Prolapse is Left Untreated?
The need for treatment depends on the severity of the prolapse. In mild cases that don't affect your quality of life, treatment might not be necessary. However, if left untreated, it can lead to chronic pain, recurring urinary tract infections and significant urinary and bowel dysfunction. The condition can greatly impact quality of life, making timely treatment essential.
How to Prevent Uterine Descent?
Preventive measures include:
- Regular pelvic floor exercises
- Maintaining a healthy weight
- Treating chronic cough and constipation
- Avoiding heavy lifting
Managing Uterine Prolapse During Pregnancy
During pregnancy, uterine prolapse is rare but can occur. It requires careful management to ensure a safe delivery. Women with prolapse should work closely with their healthcare provider throughout the pregnancy.
Can Uterine Prolapse Happen Again?
Yes, uterine prolapse can recur especially if the underlying causes are not addressed. Maintaining pelvic floor strength and following medical advice can help prevent recurrence.
By understanding uterine prolapse in women, recognizing the symptoms, and seeking appropriate treatment, you can manage this condition effectively and improve your quality of life.