Cervical cancer is one of the few cancers that’s almost totally preventable. It comes down to avoiding human papillomavirus, or HPV, which is sexually transmitted. It is the fourth most common cancer in Women. It can be eliminated, with a comprehensive approach to prevent, screen and treat.
When diagnosed, cervical cancer is one of the most successfully treatable forms of cancer, as long as it is detected early and managed effectively.
Prevention of Cervical Cancer
HPV is the top cause of cervical cancer. But it doesn’t always cause the disease. Many people have HPV and don’t develop cervical cancer.
If you’re sexually active, keep up with your doctor appointments. Your Pap or HPV tests can find abnormal cells in your cervix before the cancer starts.
Cervical cancer screening includes:
- Pap test : The sample is examined to see if abnormal cells are present.
- HPV DNA test(for some woman) : The sample is tested for the presence of 13-14 of the most common high-risk HPV types
Note : Both tests use cells taken from the cervix.
In a Pap test, your gynecologist will take a sample of your cervical cells to look for ones that could become cancer. Those “precancerous” cells might never become a problem. But it’s best to find out and get rid of them to be safe.
The U.S. Preventative Services Task Force (USPSTF) recommends that starting at age 21, women should get a Pap test every 3 years until age 65.
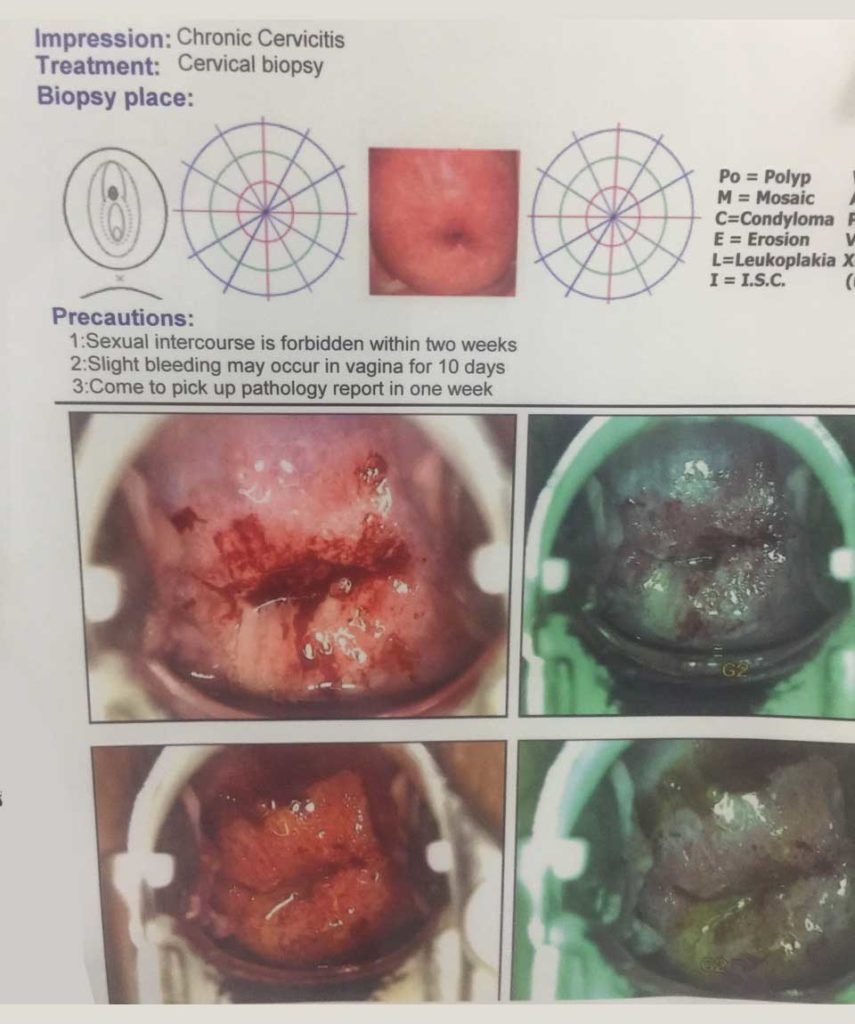
A colposcopy is a simple procedure that lets your doctor get a good look at your cervix. The exam takes 5 to 10 minutes, and is a lot like getting a Pap smear. One of the biggest differences is your doctor uses a special magnifying instrument called a colposcope.
Why is cervical cancer screening done
- helps to detect cervical cell changes before these become cancer. usually takes 3-7 years for high-grade changes in cervical cells to become cancer.
- high-grade cell changes can be removed.
- low-grade changes can be tested more frequently to see if their cells go back to normal.
Potential Benefits of Screening
- Reduced mortality and morbidity from disease, and in some cases reduced incidence
- More treatment options when cancer diagnosed early or at a pre-malignant state
- Improved quality of life
- Peace of mind
Possible Harms of Screening
- Anxiety about the test
- False-positive results
- Psychological harm
- Labeling due to negative association with disease
- Unnecessary follow-up tests
- False-negative results
- Delayed treatment
- Over-diagnosis and over-treatment
Treatment of Cervical Cancer:
With both the colposcopy and the cervical biopsy, you should be able to go back to work or school right away. But don’t put anything inside your vagina — tampons, creams, etc. — and don’t have intercourse for at least 48 hours after your biopsy.
Risks:
Colposcopy is a routine procedure, and complications are rare, though you might be sore afterwards.
Your doctor may apply a liquid bandage to your cervix after the procedure to stop any bleeding. If she does, you might have brown or black vaginal discharge. It may even look like coffee grounds. Don’t worry—it should clear up in a few days.
But call your doctor right away if you show any signs of infection, such as:
- Fever of 100.4 F or higher
- Heavy, yellow, stinky vaginal discharge
- Severe pain in your lower abdomen that isn’t relieved by over-the-counter pain relievers
- Vaginal bleeding that lasts more than 7 days
There’s always a risk that test results are incorrect. It’s rare, but it happens. And there’s a chance that abnormal cells can come back, even after your doctor removes them. That’s why it’s important to continue to get regular Pap smears and check-ups.
HPV Vaccine
- Three vaccines-bivalent (Cervarix), quadrivalent(Gardasil), & Gardasil 9
- Injected in 3 doses over 0, 1-2, 6 months(>15yr)
- Injected in 2 doses over 0, 6-12 months(9- 14yrs)
- Provides best protection if received prior to HPV exposure